TORONTO - The federal Conservatives say they're open to requiring pharmaceutical companies to publicly report gaps in their drug supply in the wake of a prescription medication shortage that caught many by surprise.
Some Canadian companies voluntarily report shortages of certain drugs, but a growing chorus of voices -- including doctors, health organizations, patient advocacy groups and Ontario's health minister -- want it to be mandatory.
"It is still a voluntary notice, so that just isn't good enough," Ontario Health Minister Deb Matthews said Thursday.
Sandoz Canada -- whose production facility in Quebec has been plagued by production issues -- only informed Ontario about the shortfall on Feb. 28, even though it knew about the problem long before that, she said.
Canada's most populous province is now scrambling to deal with the problem because Ottawa didn't give it enough warning about a slowdown in production, she said.
"We did not get the advance notice that we should have received," Matthews said. "It is the responsibility of the federal government to make sure that we're aware of slowdowns in production in time to actually prepare a response to that."
The minister wrote to federal Health Minister Leona Aglukkaq on Tuesday about the shortage, urging her to take action now to locate alternative supplies of the affected drugs.
"This drug shortage is a significant concern to me, as it threatens to cancel surgeries and delay treatment, putting the well-being of Ontarians at risk," Matthews wrote.
A spokesman for Aglukkaq accused Matthews of "playing politics" by blaming the federal government for the shortage.
Ministers from other provinces and territories have contacted Aglukkaq to talk "constructively" and work together on a plan to deal with the issue, said spokesman Steve Outhouse.
While the government still believes a voluntary reporting system is the quickest way to get information to patients and doctors, it is open to other options, he said.
"We're really concerned about how Sandoz has handled this situation, and if a voluntary approach isn't what ultimately gets this information into the hands that need it, we are open to other solutions, including regulation," Outhouse said.
The provinces could also force sole-source drug providers to notify them if there's a shortfall and penalize them if they have to buy more expensive drugs to meet demand by writing it into their contracts, he added.
Health ministers from all the provinces and territories were to discuss the drug shortage Thursday afternoon in a conference call.
Ontario's hospitals are already working together to share drugs, Matthews said.
"At this point, we have enough supply," she added. "But we do anticipate in the future that we're going to have problems, so we're working very hard to manage that now."
Matthews said she doesn't know when Ontario may run out of certain drugs because the province is still trying to determine its inventory.
British Columbia has also warned that elective surgeries may have to be cancelled if supplies of painkillers continue to run low.
B.C. Health Minister Mike de Jong said Wednesday that Sandoz's supply issues have resulted in lower stocks of routinely used injectable narcotics at hospitals such as morphine, hydromorphone and fentanyl.
It won't affect emergency treatments, life-saving procedures or the needs of palliative care patients, he said.
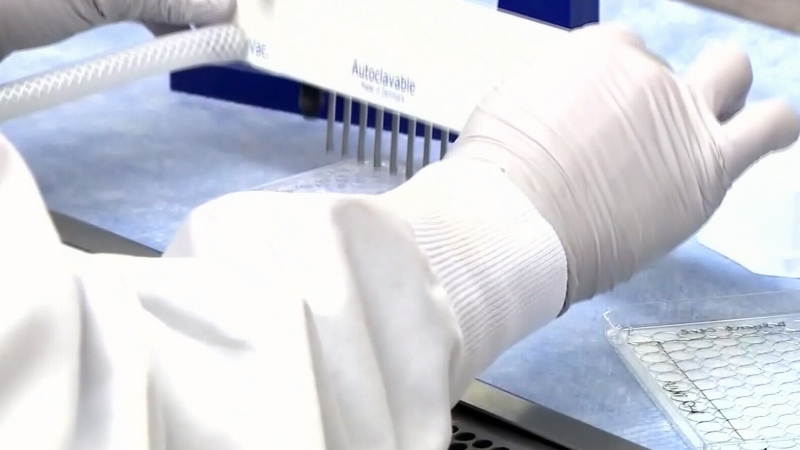
Sandoz, which is the sole Canadian supplier of many essential medications, told hospitals and other clients in mid-February that it was partially closing its plant in Boucherville, Que., while it improved its process to meet U.S. safety standards.
It halted production of several product lines and continues to produce only high-priority drug products at a reduced rate, said Matthews.
The drugs that may be affected by the production disruptions include morphine, codeine phosphate, nitroglycerine, phenobarbital, diazepam, lorazepam and testosterone.
Earlier this week, Health Canada said the federal government will speed up the approval of offshore medications as long as they meet regulatory standards for quality and effectiveness.
Experts say there are any number of reasons driving the periodic shortage of some medications, from an inability to access raw ingredients to the growing global demand for drugs.
But there is widespread speculation that some manufacturers may be choosing to reduce or even discontinue production of less profitable generic drugs in order to boost sales of newer, more expensive brand-name drugs.