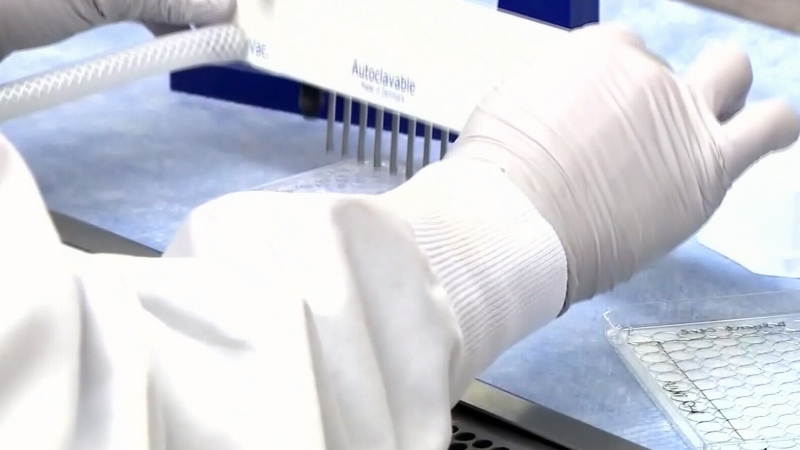
Canada needs a comprehensive national strategy to curb rampant overprescribing of opioids and to reduce escalating numbers of deaths caused by overdoses of the powerful narcotics, addiction experts say.
Writing in Monday's edition of the Canadian Medical Association Journal, Dr. Benedikt Fischer of the Centre for Addiction and Mental Health (CAMH) and co-authors say an estimated 2,000 Canadians died from opioid overdoses in 2015, and many provinces are on track for an even higher number of deaths in 2016.
"It's a real public health disaster," Fischer said in an interview. "Over the last 10 years, we're looking at somewhere between 10,000 and 20,000 dead people in Canada just from opioid overdoses alone."
In a separate report Monday, the Toronto centre urged Ottawa to launch a review of all prescription painkillers sold in Canada and said high-dose opioid medications should be pulled from the market.
Worldwide, Canadians are the second-highest consumers of prescription opioids like oxycodone, hydromorphone and fentanyl, after the U.S.
"We have hundreds of thousands of people now who are dependent on these drugs because of misuse or overprescribing or excessive exposure," said Fischer, laying the blame on the medical system that sees too many physicians prescribing the drugs for chronic pain, when research "clearly shows" it is not efficacious for that kind of pain and can actually do harm.
Medical evidence suggests opioids should be restricted to patients with acute pain, such as that related to cancer or following surgery, and should be given in limited doses and for a short duration to prevent dependence, as well as accidental overdoses.
But instead of focusing on overprescribing -- the major driver of opioid misuse and abuse -- Fischer said governments and the medical system have instead tinkered with downstream effects, such as increasing access to naloxone, a drug that can reverse an opioid overdose, and treatment of dependency with another medication called suboxone.
While Ontario has delisted Oxycontin on its provincial drug benefit program, that move merely shifted the problem to other prescription opioids like morphine and fentanyl patches, said Fischer.
However, the Ontario government announced in July it would remove those high-dose opioids from its insurance plan next year, except for patients requiring the medications for palliative care.
"Regulators and authorities have been watching this problem not just unfold but grow and get worse and worse, and didn't really take effective action," said Fischer.
Other recommendations in the report, co-authored by Jurgen Rehm of CAMH and Dr. Mark Tyndall of the University of British Columbia, include:
-- Developing and enforcing guidelines for prescribing opioids only in exceptional cases, in which there is strong scientific evidence for their use.
-- Prescribing opioids in limited dosages and for a limited duration.
-- Establishing real-time electronic prescription monitoring systems across Canada that physicians and pharmacists would have to consult before prescribing or dispensing the narcotics.
"It is late -- but not too late -- to move toward reducing the toll of opioid overuse and abuse in Canada," Fischer said.
He noted that illicit fentanyl pills from China and Mexico that increasingly are being trafficked on the street in Canada -- and have been responsible for numerous overdose deaths, particularly in B.C. -- have been a distraction from the domestic crisis created by excessive prescribing of medical opioids, which often are diverted to recreational users.
"The fake fentanyl is filling and fuelling the demand that our medical system has created," he said, adding that a national strategy needs to deal with prevention as well as treatment for the thousands of Canadians who have become dependent on the drugs.
The federal government is holding a national summit on opioids in Ottawa on Nov. 18, which will include addiction experts and organizations such as CAMH.
At the time of the summit's announcement in July, federal Health Minister Jane Philpott agreed the problem of overprescribing and opioid-related deaths has continued to worsen over the last several years.
"There's a very wide range of organizations that need to be involved in order to address the problem from the point of view of prevention and treatment," Philpott told The Canadian Press at the time.
In a related CMAJ commentary Monday, Drs. M. Eugenia Socias and Keith Ahamad, researchers at the B.C. Centre for Excellence in HIV/AIDS, say changing prescribing practices may help protect patients in the future.
"However, we're in the middle of an opioid overdose epidemic due to untreated addiction.... We need to act now: Canada can no longer afford to be a witness to this devastating epidemic," they write, suggesting that Canada adopt a plan similar to the National Pain Strategy in the United States.