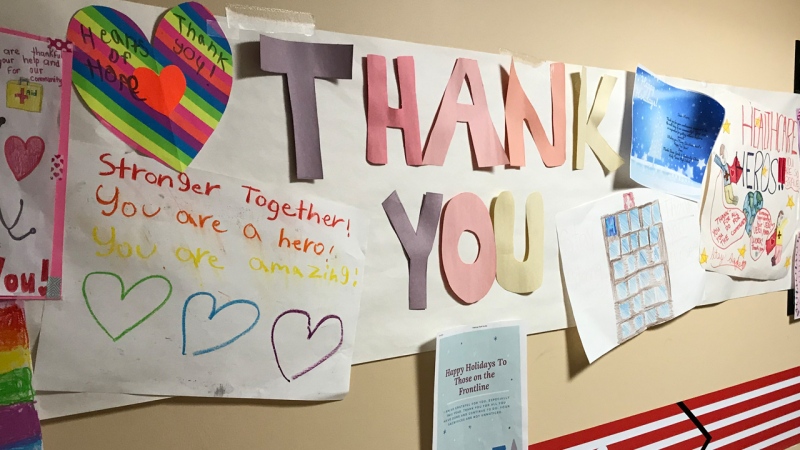
CAMBRIDGE -- The fight against the novel coronavirus is far from over at Cambridge Memorial Hospital.
That was the message from those on the front lines, as CTV News got an inside look at the hospital’s new intensive care unit, which opened only weeks before the onset of the pandemic.
“We are in the fight of our life right now, and I know with things improving it seems like we are at the end of this, but we are in the fight of our life,” said Dr. Jonathan Marhong, CMH’s Medical Director of Quality and Patient Safety, who has been on the front lines of the battle against COVID-19 for months.
“Things can go from being business as usual to being life-threatening, dangerous, and tragic at the same time,” he said.
The ICU was bustling with nurses, doctors, and respiratory therapists, all wearing extensive personal protective equipment.
The rooms are equipped with specialized doors and barriers that Marhong says prevent the virus from spreading.
“We have everything that we need to take care of the sickest patients in the region,” said Dr. Marhong.
Cambridge Memorial Hospital experienced a peak of 14 COVID-19 positive patients in early to mid-May, with only a few being treated in the ICU.
The normal ICU capacity is 12 beds, but the area can surge to accommodate 22, with overflow available in other areas of the hospital if needed.
“We have seen the numbers trending downward,” Dr. Marhong said. “There have been some occasional spikes in the region, but overall it seems like things are fairly reassuring.”
But as the economy reopens, Dr. Marhong believes another peak is on the way.
“We have seen that time and time again with a lot of pandemics and epidemics,” he said. “The possibility is very distinct and we are ready for it.”
PREPARING FOR THE FIGHT
As COVID-19 began spreading throughout Canada back in the early months of 2020, hospital staff spent countless hours preparing a pandemic plan.
“It was very difficult to prepare because we didn’t really know what was coming,” said Dr. Marhong. “It was a virus that was new, we knew that it was dangerous, and it was highly contagious.”
Dr. David Cape is an intensive care unit doctor at the hospital. He said at the start of the pandemic, there was a lot of anxiety about the unpredictable illness.
“We talked to other physicians across the province, we learned about best practices in centres hit hard by COVID-19, like New York City and Northern Italy,” he said. “We had multiple meetings, workshops, and training simulations.”

The hospital expanded ICU space, brought in more ventilators, and determined a plan for use of different types of personal protective equipment, like surgical masks or N95 masks.
“We have come to rely on each other as a team,” said Dr. Cape. “It has been formative for the doctors, nurses and respiratory therapists.”
“I felt like I was going to war,” said Dr. Marhong. “I felt like there was a sense of responsibility to society, to my patients, to someone who is sick and may not have somebody to care for them. And I say to myself, we need to be at the bedside.”
SHIFTS, SACRIFICES AND STRESS
A typical work day for ICU doctors working at the bedside of patients at Cambridge Memorial Hospital is an 11-hour shift.
They say the biggest risk factor is minimizing exposure and potential spread of the virus.
“The exposures that are most concerning are when we are intubating a patient, so placing them on a ventilator,” Dr. Marhong said.
The process of intubation means inserting a tube into the larynx, an organ in the neck that is involved in breathing and producing sound.
That tube is then secured to a ventilator, but the process aerosolizes airway secretions, meaning it disperses COVID-19 into the air.
Medical staff wear personal protective equipment and typically perform these types of procedures in specialized negative pressure rooms, where air is constantly re-circulated.
But these types of exposures have still required Dr. Marhong to isolate himself from his family twice for a period of 14 days.
“I would see my daughter and my wife sort of out of the doorway or out the window as they played in the backyard,” he said. “It was hard”.
Dr. Marhong described the pandemic as the most challenging phase of his career.
He said there’s been constant stress about potentially bringing the deadly disease home to his two-year-old daughter, or spreading the virus to patients and colleagues.
“It’s led to many tearful conversations before I go to work, which has been hard to work through,” he said. “The balance came when we said to ourselves, well this pandemic can last 18 to 24 months or even excess to that, depending on how many waves there are. It’s not like I can avoid seeing my daughter until she’s four years old.”
He said his family has compromised with hand washing, cleaning surfaces, and being very careful with hugs and kisses.
CHALLENGES: MEDICAL AND EMOTIONAL
Dr. Marhong said a majority of patients in the ICU with COVID-19 are in their 60s or 70s, with many having underlying medical conditions.
“It’s very unpredictable, they all follow their own timelines when they become critically ill,” he said. “For some reason, this virus interacts with them in a way that makes their heart, lungs, and even their core systems within the brain, very unstable.”
He said doctors have had to throw away the textbook and roll with the punches.
COVID-19 can cause a large inflammatory response in the lungs that cause the oxygen levels to go down and breathing to fail, he said.
He said the virus can also cause the heart to fail or weaken.
“Their heart rate may be really fast at one point, but really slow at another point,” he said. “We have to really shuffle to shift our medical approach to accommodate that.
“I tell this to families all the time, things change minute to minute. The status of their loved one can change within the blink of an eye,” said Dr. Marhong. “A lot of these patients are very unstable all the time and very resistant to the therapies that we provide.”
He said it’s also heartbreaking to see family members who can’t be by the bedside of their loved ones.
“They have to make life-altering decisions about their family member knowing that they may have a major surgery or a major maneuver on the ventilator that may be life-threatening,” he said. “That may be the last time that they hear about their family member. It’s very difficult and I share with them that I can’t imagine the pain that they are going through.”
LONG ROADS TO RECOVERY
There are still a lot of unknowns about the lasting effects of COVID-19 on the lungs or other body functions.
“When they do become critically ill, they do tend to be in the ICU for a much longer period of time,” said Dr. Marhong. “They do tend to require the ventilator for a longer period of time.”
After being critically ill in the ICU, there is also a road to recovery for COVID-19 patients.
“They suffer things like weakness and reconditioning,” he said. “Trying to get them to take their first steps. It’s not always the case that we have a happy outcome for these patients.”
Dr. Marhong said no patients have died from the virus within the ICU, the vast majority have gone home with some requiring additional mobility help.
“I think that a lot of the patients that come through the ICU that have experienced the devastations of COVID, do struggle to get back to their quality of life,” he said.
PREPARING FOR WHAT’S NEXT
Waterloo Region is more than 100 days into the pandemic.
“All we can do is prepare, said Dr. Cape. “Our assumption is COVID is here to stay for the time being, but in terms of what will happen depends on a lot of questions that we don’t have the answer for and of course, a vaccine development.”
Dr. Marhong thinks the epidemiologists are right in saying that the fall is a season when the public should be concerned.
“I would say don’t let your guard down,” he said. “Be careful, enjoy your life and do what you have to do, but as things open up I would say: hand hygiene, don’t touch your face, physical distancing, and wear a mask.”
Dr. Marhong says staff at Cambridge Memorial Hospital will be prepared no matter the outcome.
“We have to be prepared,” he said. “We will be prepared and we will provide care and we will be at the bedside. Nobody is going to run away. We are going to win this. We are going to win this together.”