KITCHENER -- A national study used Kitchener-based technology to prove ‘remote patient monitoring’ post-surgery has many benefits for both patients and physicians.
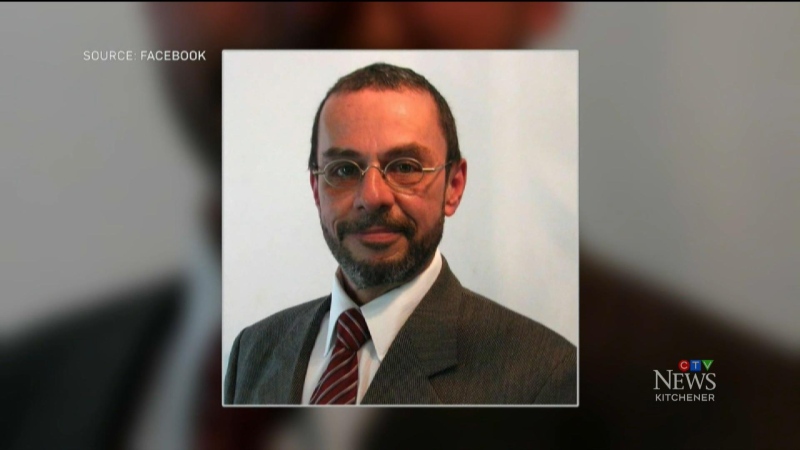
The study, called ‘Post discharge after surgery Virtual Care with Remote Automated Monitoring technology-1’, or ‘PVC-RAM 1,’ was led by Hamilton-based researchers Dr. PJ Devereaux and Michael McGillion.
The study included 900 patients, and evaluated if ‘remote patient monitoring’, or RPM, when used for 30 days post-surgery, improved patient outcomes compared to standard care, where the onus is on the patient to seek healthcare support.
Patients took home Kitchener-based company Cloud DX’s Connected Health Kit to monitor their vital signs at home, including heart rate, blood pressure, oxygen saturation, respiration rate, body temperature and weight.
Nurses are also able to check in with their patients using the technology and patients can send their nurse or doctor photos of their surgical wounds and virtually access a nurse or doctor 24 hours a day.
“There’s been no intervention where I’ve received so much spontaneous feedback from patients, about saying how crucial it is to make sure this technology is available to people in the future,” said Devereaux.
“Doctors prescribe ‘Connected Health’ to patients after their surgery,” said Robert Kaul, the CEO of Cloud DX. “Patients take a kit home with them that includes a tablet computer and medical devices, that are licensed by Health Canada, to gather their vital sign data.”
Ernie Seeger was diagnosed with cancer earlier this year. After his surgery, he took part in the study, and enjoyed having virtual care at his fingertips.
“They would call us every night at a certain time,” said Seeger.
“I personally think it should be handed to people as they’re walking out the door from their surgery, like a gift bag,” Seeger added with a laugh. “It was awesome, and so easy to use.”
Seeger recalls one night he was in a lot of pain and was able to get in contact with a doctor late at night. “I called the service in place, and the doctor automatically knew exactly what was going on.” Seeger said. “He wrote me a prescription and I was able to pick it up the following morning, before 11 o’clock on a Sunday”.
The results of the study revealed virtual care reduced patient pain, and could reduce hospital readmissions and emergency care visits.
Researchers found virtual care also resolved and prevented drug errors during patient care transition.
“Through the virtual care process, we identified that 30 per cent of patients went home with drug errors, and on average, two drug errors,” said Devereaux. “In standard care, only six percent of those drug errors are detected.”
Devereaux says he was surprised the drug error was that high.
“It just highlights why we need a different system to mitigate that problem,” said Devereaux.
Following the PVC-RAM1 study using Cloud DX’s technology, Hamilton Health Sciences adopted the model and is currently using this type of care in its surgical transitions program.
There are plans to take the research even further.
“We’re getting ready to start the PVC-RAM 2 trial,” said Devereaux. “We will expand and better figure out how to make these interventions more efficient and effective.”